Meet the woman taking maternal mental health by storm
Recently I had the distinct pleasure to meet with my friend Kim Kertsburg, LCSW of Dallas Postpartum Support. As part of my blog series featuring Dallas business owners who serve families with young children, it was an honor for me to meet with an actual hero. Kim provides counseling to women who are experiencing mental health complications such as depression, anxiety, or adjustment issues during pregnancy and postpartum. Her work is invaluable to our community. I hope you enjoy reading along with this interview to learn more about this extremely important issue. You can read more about my series on businesses here in Dallas and my mission to bring the best resources to parents in Dallas and why it is important to me as a newborn photographer.

Kim: Well let me just start out by saying I am a Perinatal Psychotherapist and have been in the mental health field for about 23 years now. I work exclusively with pregnant and postpartum women who have any sort of depression, anxiety or adjustment issues. Our mission statement at Dallas Postpartum Support is to provide cutting edge assessment and treatment for pregnant and postpartum women with perinatal mood and anxiety disorders.
I also do a lot of speaking engagements throughout the DFW area to spread awareness and train first responders such as midwives, doulas, OB’s and nurses.
Laura: So perinatal refers to the time when you are pregnant and afterwards?
Kim: Correct. The term perinatal refers to the time encompassing the entire pregnancy and one year postpartum. Interestingly enough, I have moms that call me and they are 15 months postpartum and ask if they could still have postpartum depression? And I say absolutely. Technically they are out of the postpartum period but some women do not get treatment for postpartum issues, so the symptoms can linger and/or get worse.
Laura: Right! Because you’re supposed to be full of joy, full of bliss!
Kim: Yes! When well-meaning people approach a new mom they ask, “isn’t this the happiest time? Aren’t you the happiest mommy?” “Don’t blink you’re going to miss it.” And it’s certainly not popular for that new mom to say, “I’m feeling really depressed. There’s something wrong with me. I don’t feel like myself. I’m having scary intrusive thoughts about harming my child. This isn’t what I expected.” That’s not popular to say at a cocktail party.
Laura: Every time you become a parent it’s a huge adjustment to your family. You have all new relationships to form. You have to shift everything and make space in all the relationships in your family. In your marriage, with your other children, and then if anything at all goes wrong – oh my gosh! I got sick after our last baby and it was just horrible! You’re so vulnerable and fragile.
What is the most common health complication of pregnancy?
Kim: I love that you brought that up. Did you know that in a woman’s entire lifetime she is at the highest risk and is the most vulnerable for mental illness during the postpartum period. When I meet with couples for a postpartum planning session, I start with statistics. That up to 1 in 5 women will experience some sort of mental health complication and that maternal mental health complications are the number one medical complication of childbearing. Perinatal women are more likely to have depression or anxiety compared to gestational diabetes, postpartum hemorrhage, preeclampsia, and several other issues that could arise. It is generally accepted that 1 in 7 women will specifically have postpartum depression. I think it might be higher than that, it could be underreported. Postpartum depression gets the most attention but it’s about the same statistic for postpartum anxiety. When you look at all the things that can happen in the perinatal period I think it’s more like up to 1 in 5. And out of that number only about 15% of women ever get any help.
What are the risk factors for perinatal mental health complications?
Laura: Are there any statistics about if a person has ever had mental health issues like anxiety or depression prior to their pregnancy and how that would increase their likelihood of experiencing a complication like postpartum depression or anxiety?
Kim: Yes. Great question. While maternal mental health complications cross all religious, racial and socioeconomic differences, there are pre-existing issues that can cause a woman to be more at risk. If a woman has a history of mental health issues or if it runs in the family tree, she is more at risk. If you are a woman of color, you are more at risk. If you have various stressors going on or lack of supports, you are at more risk. If you had previous miscarriages or losses, had infertility issues or treatment, have struggles breastfeeding or if you had a traumatic birth, you are more at risk. Not just about depression but a spectrum of other things that can happen. Which are perinatal depression, anxiety, panic disorder, PTSD – either related to past trauma or birth trauma, OCD, and psychosis. Those are all the things – that’s what I call the 1 in 5. Also, related to PTSD, if you have any sort of history of abuse or childhood sexual abuse or a time when you felt vulnerable, powerless and didn’t have control over things that were done to your body you can have complications from those things. Even if you feel like you’ve recovered from past trauma, symptoms can resurface. Why? Because there is nothing predictable about pregnancy, labor and delivery and the postpartum period. You really don’t have control over your body and you have various people touching you. You may experience pain, confusion and vulnerability. It can stir up a lot of those old memories.
Laura: I think too, many of us didn’t experience the ideal parenting situation. I think that even just becoming a parent and having to look at how you are going to parent and then dealing with your significant other and how they want to parent and having to decide that together. Doesn’t matter how many talks you had about it before…
Kim: or the 20 books you read about it
Laura: laughs
Kim: I think, understandably so, expectant parents spend so much time on pregnancy, labor and delivery, there is almost zero preparation time or thought given to the postpartum period. I love working with couples that make appointments for postpartum planning. I help them troubleshoot and navigate through what is going to happen after the delivery.
Laura: What about PMS?
Kim: (nods) If you are sensitive to hormone changes that increases your likelihood that something could happen. Your progesterone and estrogen levels are just skyrocketing while pregnant. And once the baby is delivered they crash. And that hormone change in addition to other risk factors is possibly why women experience mental health complications.
Laura: You know what I kind of liken it to, and this is maybe simplifying it too much, and I don’t mean to diminish it, it’s the way that I feel about the way we react to any situation. If you’re hungry, tired, sick, uncomfortable, or feeling any of those things it makes any situation worse. It makes your capacity to deal with that situation that much less. So you’re talking about adding stress factors. The more stress factors you have, the more at risk you are.
Kim: That’s absolutely correct! So some clients or their partners will call me and say, “my wife is not herself. I don’t know what’s going on and we just need some help.” Here is a common scenario that I experience: A woman calls me and says she is really worried about the anxiety she is feeling. She reports she was a perfectionist for most of her life. She’s a lawyer, very high functioning. Maybe a little anxiety here or there in the past. Moves from New York to Dallas. Can you see how it’s layering up already? Her family is all in New York, she don’t know anyone here – isolated. Her husband travels a lot. Not a lot of support at home. Let’s say that she was ill for the first 6 months of her pregnancy. Didn’t go as planned. She has baby. Baby’s a couple weeks early and had to go to the NICU. So she’s pumping, trying to feed baby. And then let’s say she tries to breastfeed baby when they’re out of NICU and it’s not going very well. Now add on that she has a baby who has to eat every two hours. She’s sleep deprived for a couple of months. You can see how easily depression or anxiety can creep in.
Where do we start to find healing?
I would say that my prescription for getting the train back on the tracks is 1) sleep, 2) nutrition, 3) exercise and 4) routine.
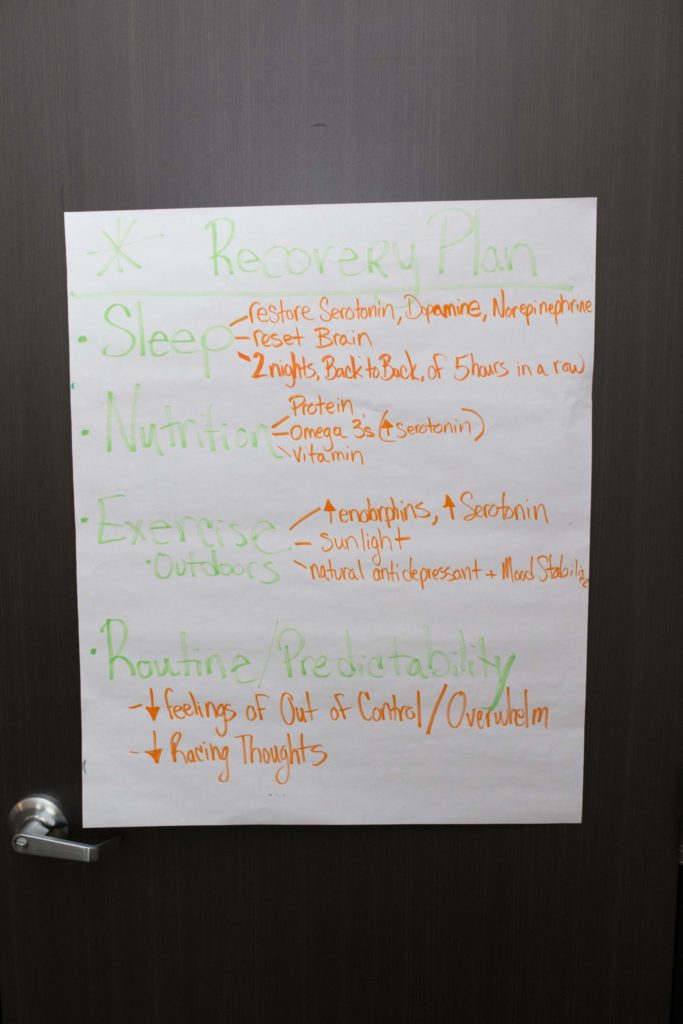
- So with sleep, we need to restore Serotonin a lot of that is restored while you are sleeping. The minimum amount of sleep that a postpartum woman needs is 2 nights back to back of 5 hours sleep in a row. That’s a goal. If you are breastfeeding or bottle feeding and you don’t have anyone to help you, this can be a difficult goal. It would be best if the 5 hours were uninterrupted. And sometimes I need to talk to partners or other family members about helping out. Because for women who are stay at home moms or working moms, they get the message – this is my job, I have to do this. And I say to families, if there are mental health complications, it is a family issue. Everyone needs to pitch in and circle the wagons.
- So nutrition. What I tell my moms is I am not the food police. If you need to have your kitkat have your kitkat. But, can you get protein in your meals? Don’t skip meals. Women who are feeling really depressed and anxious, they’re not going to feel very hungry. Or they’re over eating. But can you get protein in your meals? Get some Omega 3s and a multivitamin
- Exercise for perinatal women. It’s not to get bikini ready. It’s not for that. We are looking at ways to increase endorphins and serotonin. I start out with basics by saying can you get outside? Can you get some sunlight on your face? I know that it is 110 degrees outside but can you at least get outside for a bit? Fresh air, sunlight and getting outside is a natural antidepressant, it can help when women are anxious and depressed. They feel trapped. And once you’re medically cleared for exercise can you walk up and down your block? If you live in an apartment building can you walk up and down the hallway? Can you walk a distance and back. And just start small. But you’ve got to move your body.
- And then routine. Women who feel overwhelmed, feel out of control, who have racing thoughts or anxiety, can you feel a bit better from routine and some sort of predictability. Why? Because you will just feel a bit more in control and have a bit more stability in your day.
Laura: Well that’s why everybody likes routines. You put some sort of structure in the day. It gives you the feeling of knowing what to expect.
Kim: Absolutely. And women today are under such pressure. Pressure to perform. Pressure to do it all. Pressure to never let them see you sweat. And I’m here to say, what’s good enough? And good enough doesn’t roll off the tongue very well. But what is good enough? We can’t do perfect. What is good enough? Because I know for women, motherhood is the single most important thing they will ever do in their lives and they don’t want to screw it up. And they need to hear, you are doing great and what you don’t know – you will figure out.
What effect does maternal mental health have on the rest of the family?
Laura: How do perinatal mental health complications affect the rest of the family?
Kim: I don’t know if you know this, but if a woman has postpartum depression there is a 50% higher likelihood that her partner will become depressed and there is a 50% likelihood that their children will become depressed by the end of their adolescence. Believe me when I say, it is a family problem.
Laura: That is a really interesting statistic. That is really interesting. Wow. My mind is blown.
Kim: Can I tell you this? Dads can have postpartum depression.
Laura: This makes sense to me. It’s an adjustment for them to. They don’t have the hormones, I mean maybe they do have some kind of hormone shift.
Kim: Yes, changes in hormones, including testosterone, estrogen, cortisol, vasopressin, and prolactin, during the postpartum period in fathers may be biological risk factors in paternal PPD. Fathers who have excessive stress from becoming a parent, lack of social supports for parenting, and feeling excluded from mother-infant bonding, may be more likely to develop paternal PPD.
Laura: How many dads will get postpartum depression?
Kim: The statistic is about 1 in 10 dads will experience postpartum depression
Laura: Shut up!
Kim: And how many do you think get help?
Laura: Zero!
Kim: Barely any. I think a dad may hesitate to seek help and admit he thinks he’s experiencing postpartum depression. If there’s such stigma and shame around it for moms, what is it like for dads? Dad’s most likely aren’t going to say anything.
What is the baby blues?
Laura: What is the difference between the baby blues and postpartum depression, anxiety or psychosis?
Kim: The baby blues is not even a mild form of depression. It is a non disorder. The statistics are about 60-80% of women will experience mild symptoms of being overwhelmed, feeling fatigued, mild mood swings (grateful, overjoyed and then crying again). The baby blues peaks at about 3-5 days postpartum and it lasts about 2 weeks and if it goes beyond that it isn’t the baby blues anymore. And if you aren’t feeling ok you need to let someone know. What’s interesting is in a typical depression, you have the excessive crying, insomnia, extreme fatigue, pervasive sadness, hopelessness, despair, worthlessness, loss of pleasure, loss of energy, feeling overwhelmed, but a hallmark symptom of perinatal depression is anxiety. So you may not be looking at a mom who’s really sad or can’t get out of bed. You may be looking at an irritable mom. You might be looking at a mom who feels rage or sad at the same time. That’s something for women that is important to know. That’s what makes it unique from a typical depression outside the perinatal time. There’s an anxiety component that looks like irritability or excessive worry.
What is postpartum anxiety?
Laura: People who experience rage are actually experiencing anxiety? Or they’re tied together?
Kim: You can be depressed and irritable, you can be anxious and irritable. But for perinatal depression there can be an irritable, anxiety component. You can have postpartum depression or postpartum anxiety separately. You can also have both.
Laura: You can have postpartum anxiety on its own?
Kim: Absolutely. Absolutely. I feel like I see more anxiety in my office than I do depression.
Laura: So what I think that is really interesting to me is that being an informed woman, being educated about all of this stuff, I wasn’t really aware of that that anxiety could be on its own. And I think, I’m not really experiencing that anymore, but I think I really should have come and talked to you before about the anxiety. And the massive irritability. Because I’ve basically been irritable for 10 years. And angry.
Kim: I know for a lot of women, symptoms can manifest emotionally and physically. They’re slamming doors and drawers. They’re scratching their arms, legs, pulling their hair out. Screaming at their loved ones. Then the guilt and shame spiral begin.
Laura: What I think is interesting to me is that has always been tied to how do you manage being upset in my family. To yell. That was the answer. That’s how you deal with overwhelming emotions. You just flip out on people. And I think worked on that and got better. It would have been great to get some help with that though.
Kim: I think one of the most important jobs I have is to normalize what women are feeling and put a name to it. Up to 1 in 5 women? That means mental health complications are common.
Laura: That’s really amazing
Kim: Women come in and have had scary intrusive thoughts about harming their child or themselves and they think they’re going crazy. And I say, that is Perinatal OCD, it has a name and there is a treatment for it. After I say this, usually I see their shoulders visibly relax. They start to believe that they aren’t bad moms, just women who have a treatable medical condition.
“…the number one medical complication of childbearing is maternal mental health complications.”
I think women need to know that the number one medical complication of childbearing is maternal mental health complications. And this is good for partners to know as well. Typically a mom is not going to go to her partner or to a friend and say, “I feel hopeless and despairing,” “I feel like killing myself,” “I am not able to shut my brain off, and I have this impending sense of doom, and I just can’t relax, and I’m having intrusive images of hurting my child.” She’s not probably going to say that to you. But what she will say to you is, “I don’t feel like myself, there’s something wrong.” That’s the red flag.
Laura: In my case, I first of all didn’t know until we’re sitting here now, I’m telling you I feel ok now, maybe a year ago the anxiety and maybe even a bit of OCD were not right. And I managed it all myself and I didn’t ever feel like that was something I could go to anyone and say anything about. I didn’t tell my husband. There was something happening with me and I needed to get myself under control. I really want to say something about that.
Kim: That is why I recommend postpartum planning for any expectant person. I help moms and partners learn symptoms to look for and how to say the right things. Because women who go to their family, friends, doctors etc. aren’t going to list the clinical symptoms of depression or anxiety. They’re going to say they aren’t feeling good, or I’m not feeling like myself. Guess what answers they get – you’re strong enough, you can do this, you just had a baby, you’re going through hormonal changes. Note to family members and partners: If she’s coming to you and telling you she feels like she’s failing at the single most important thing in her life, she’s already been strong enough. And she’s coming to you with probably a lot of guilt and a lot of shame. And she’s saying “I don’t quite feel like myself,” so this is what you say, you say, “I believe you, I’m glad you told me, I’m concerned too, let’s find some help.” That’s all you need to say. You need to hug her and tell her she’s doing a great job. Tell her, “you’re a great mom.”
You can be symptomatic and competent at the same time. You can be a depressed or anxious mom and still be a great or competent mom. You just might need some help. I tell moms and partners, trust your instincts, if you feel like something is off or wrong it probably is. Let your OB know, let your midwife know, let your partner know. Don’t stop until you get some help. If you are experiencing some sort of mental health complication it is not a moral weakness, it’s not a defect in character, it’s not your fault, you’re not to blame, this stuff is so treatable. With help you can and will get better. I make sure women do not leave my office until they have a sense of hope. I let them know, I know how to treat this illness, I’m not afraid of the dark. I will look them in the eyes and say I know what this is. Here’s the name of what you’re going through. It is a medical condition. And honestly help is usually a relatively short amount of time. I would say on average I see women anywhere from 2-5 months. So we’re not looking at years of therapy. I’m very solution oriented. Let’s take a look at your symptoms, let’s get your symptoms managed and under control. Let’s get to the core root of the issue, which is usually some kind of distorted thought or belief like I’m worthless, I’m not enough or I’m a bad mom. We treat the negative thought patterns and then women feel better. I will do this for the rest of my life.
How is postpartum psychosis different?
Laura: What about postpartum psychosis?
Kim: Postpartum psychosis is relatively rare. It occurs in 1-2 women in a 1000. Typically it requires inpatient treatment for stabilization. Women have a break with reality and have psychotic symptoms like auditory or visual hallucinations, delusional/bizarre thoughts, disorganized thoughts and speech to name a few symptoms. Postpartum Psychosis has a high suicide rate and high infanticide rate. It requires hospitalization and usually medication.
Laura: Do we have good resources in Dallas for hospitalization or are we still working on it?
Kim: We’re still working on it. The SEAY Center Texas Health Resources in Plano, and then also in Allen there is a 12 bed inpatient for women only. It’s not specifically for maternal mental health but at least it is for women only. One of the closest inpatient perinatal place for women to go is North Carolina.
Even women who were in therapy for a long time prior to pregnancy, they think – I’ve got this. I have all of these coping skills, I know how to handle things. But the perinatal period is completely different. Why? The stakes are higher. You have a human being to take care of. You have a complete shift in identity. You have gone from someone who probably had a lot of freedom, could go to Starbucks whenever you wanted, went out to the movies with your partner, and did all of those things and stayed up until 12:00 and slept in until 10:00 on the weekends. And had a career.
Laura: We used to joke that our lives ended when we had our first. We were reborn as parents. Because we became completely different people with a completely different focus.
Kim: For some women though, they need some help bridging the old life they knew to the new life they have. Moms sometimes have to grieve their old life and who they used to be and redefine who they are today. I have so many women who come to session and say I don’t know who I am, I don’t know where I’ve gone. And I say the good news is that you get to redefine who you are today, you get a blank slate. You probably won’t go back to who you were because you are a mother now, you have a child now. But can you be bigger, better, faster, stronger? You bet you can.
Laura: I think my children have made me. They’ve made me into just a much better human.
Kim: What I know to be true, is that the women that I work with are some of the most courageous, hilarious, brave and strong women that I have ever met. I want to make sure that is said. These women are seeking help for something that has such shame and stigma. Some moms do not seek therapy for themselves, but they will for their children. They want to be better for their kids. I have been moved and humbled by the stories that they tell. By the vulnerability and just their willingness to be open about their most dark time in their entire life. And they share that with me. And I am honored by that. And that’s why I will do this for forever. These women, I have such respect for them. And I have the privilege of watching them heal and soar.
If you or anyone you know is struggling with perinatal depression, anxiety, or any of the things discussed in this article, please reach out to a loved one, a health professional and/or Kim. She is there to help and support you and get you through this time. You can reach Kim at 214-300-5333 and Her website is Dallas Postpartum Support.









12 Responses
Wonderfully written! thank you for helping others to understand this issue and those who struggling through it!
Momma’s health is very very important. Thank you for writing this and bringing awareness!
I think it’s wonderful that you’re using your platform to bring awareness to this! Mamas are fulltime caregivers, and need care themselves.
What a great read! It’s so good to know that we are not alone in this a new mothers. Thank you for bringing attention to a subject that’s not usually discussed!
What a great resource for new moms.
Great interview! Wonderful resource for such a vulnerable time.
I love that you are shedding light on maternal health. I struggled with really profound depression after my preemie was born and in the NICU. I think it took a whole year for me to come back into myself, and I had a lot of help. Dallas is really lucky to have such a wonderful resource for women.
So great to spread awareness!
Wow, what a powerful post that hit very close to home. As someone who didn’t suffer from postpartum depression until around 3 months after giving birth, I was completely unaware of what I was going through, and just thought I was losing my mind. Thank heavens I had a great support system around me. As a newborn photographer, it is great to see you shedding light on such a serious topic for women going through pregnancy and childbirth. Dallas is lucky to have another resource to go to not just for newborn portraits but for support. Keep up the great work!
I am so glad this resonated with you. Thank you so much for your comment. When we talk about it it releases the stigma and more women can get the help they need.